Blood Sugar After Meals: What's Normal?
Think of your blood sugar after eating as your body's "metabolic report card." It tells you how efficiently your system processes food, especially carbs. After a meal, your blood glucose rises naturally. But if that spike is too high—or stays elevated too long—it can signal trouble. Whether you're managing diabetes or just trying to stay healthy, tracking post-meal sugar helps you avoid fatigue, inflammation, and long-term health risks.
High postprandial glucose (PPG) is more than just a temporary spike—it’s linked to increased risk of heart disease, nerve damage, and even cognitive decline. It’s like a silent alarm your body rings to say, “Hey, something’s off here.” Catching that early and making changes can mean the difference between thriving and developing serious conditions later.
Your body ideally wants to return your blood sugar to normal within two to three hours of eating. If it doesn’t, your insulin response could be sluggish—or you're consuming foods that are difficult for your system to process. Either way, understanding this helps you fine-tune your meals, activity levels, and habits.
How Blood Sugar Is Affected by Meals
When you eat, especially foods rich in carbohydrates like bread, pasta, or fruit, your body breaks them down into glucose. This glucose enters your bloodstream and causes your blood sugar level to rise. In response, your pancreas secretes insulin, a hormone that helps transport glucose into your cells for energy or storage.
But here's the kicker—not all meals are created equal. A meal packed with refined carbs and sugar will spike your blood sugar fast and high, then potentially crash it down just as quickly. Balanced meals that include fiber, fat, and protein slow the digestion process and reduce this spike, keeping your glucose curve more like a rolling hill than a sharp mountain peak.
Other things also affect how your body responds—your insulin sensitivity, activity level, even how much sleep you got last night. It's a complex dance between your food choices and your metabolic system.
What Is Considered Normal Blood Sugar After Eating?
Standard Ranges After 1, 2, and 3 Hours
So, what’s the “magic number” when it comes to blood sugar after meals? While targets can vary slightly depending on your health status, here are general post-meal glucose goals:
-
1 hour after eating: under 140 mg/dL for non-diabetics, under 180 mg/dL for diabetics
-
2 hours after eating: under 120 mg/dL for non-diabetics, under 140 mg/dL for diabetics
-
3 hours after eating: approaching fasting level (70–99 mg/dL for most people)
These figures help indicate whether your body is efficiently managing glucose. If your levels stay elevated after 2–3 hours, it may suggest insulin resistance, poor food choices, or even early signs of metabolic syndrome.
But context is key. Let’s say you had a big pasta meal, and your 1-hour post-meal reading is 155 mg/dL. That might not be cause for alarm, especially if it returns to normal within 2–3 hours. But if it lingers around 160 or 170 after 3 hours, that's a red flag worth investigating.
Differences Between Normal, Prediabetic, and Diabetic Ranges
Understanding these ranges can help you figure out where you stand:
| Condition | Fasting Glucose | 2-Hour Post-Meal |
|---|---|---|
| Normal | 70–99 mg/dL | < 140 mg/dL |
| Prediabetes | 100-125 mg/dL | 140–199 mg/dL |
| Diabetes | 126+ mg/dL | 200+ mg/dL |
If you're consistently seeing post-meal numbers in the prediabetic or diabetic range, it’s time to take action. That might include revising your diet, getting more exercise, or consulting your doctor. The good news? Postprandial glucose is something you can control, often with just a few strategic lifestyle tweaks.
How the Body Regulates Blood Sugar Post-Meal
Role of Insulin and the Pancreas
Imagine insulin as the key to unlocking your body’s energy vault. When you eat, your pancreas kicks in, releasing insulin to help shuttle glucose into cells. If the pancreas doesn’t produce enough insulin—or your cells resist it—sugar stays in your bloodstream too long, leading to those concerning post-meal spikes.
For most people, the pancreas does its job quietly. But in people with diabetes or insulin resistance, the mechanism breaks down. Either insulin production is insufficient (as in type 1 diabetes), or the body becomes resistant to it (as in type 2 diabetes). In both cases, postprandial blood sugar regulation gets thrown off track.
Even healthy individuals can experience occasional insulin lag—maybe due to poor sleep, stress, or an unusually high-carb meal. That’s why tracking is so powerful: it provides real-time feedback on how your lifestyle affects your glucose response.
Glycemic Response and Digestion Time
Your blood sugar response to a meal isn’t just about what you ate—it’s also about how your body digests it. Some foods break down quickly, flooding your bloodstream with glucose, while others digest slowly, releasing sugar more gradually.
The glycemic index (GI) helps predict how different foods affect blood sugar. High-GI foods like white bread or soda spike glucose levels rapidly. Low-GI foods like beans, oats, or sweet potatoes lead to a gentler rise.
Digestion time also matters. Meals rich in fiber and fat take longer to break down, which slows glucose absorption. That's why a mixed meal (protein + fat + carbs) usually leads to a more stable post-meal blood sugar curve than carbs alone.
Factors Influencing Post-Meal Blood Sugar Levels
Meal Composition (Carbs, Fats, Proteins)
Here’s a truth bomb: not all calories are equal when it comes to blood sugar. A 300-calorie plate of cookies hits your bloodstream very differently than 300 calories of grilled chicken and quinoa.
Carbohydrates, especially refined ones, have the biggest impact. They digest quickly and turn into glucose fast. Proteins and fats, on the other hand, have a minimal effect on blood sugar. In fact, combining them with carbs can blunt the sugar spike. For example, adding avocado or nuts to toast slows down how fast sugar hits your blood.
Fiber is another game-changer. It adds bulk and slows digestion, helping keep sugar levels steady. That’s why whole grains, fruits with skin, and veggies are better choices than processed or juiced options.
Understanding this can help you build meals that work with your body, not against it.
Timing and Size of Meals
Ever wonder why you feel sluggish after a big lunch? Oversized meals can overload your digestive system, leading to a steeper and longer-lasting glucose spike. Smaller, more frequent meals help keep your blood sugar more stable throughout the day.
Eating late at night is another culprit. Your body’s insulin sensitivity dips in the evening, meaning that same plate of pasta will spike you higher at 9 PM than it would at noon. That’s why dietitians often recommend having your largest meal earlier in the day and tapering as evening approaches.
Meal timing and size are like the tempo of a song. Get it wrong, and everything feels off. But when you sync your meals to your body's rhythm, your energy and metabolism stay in harmony.
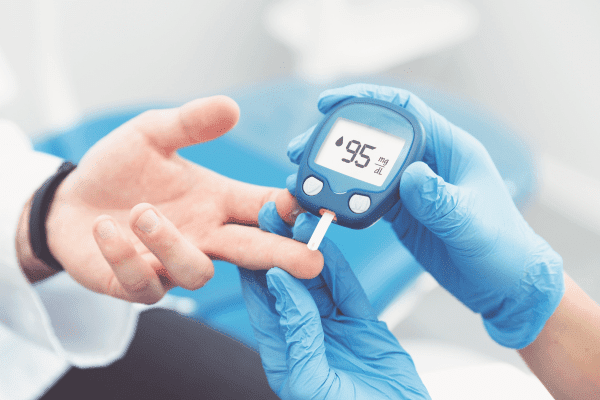
Tools for Monitoring Blood Sugar After Meals
Glucometers and Continuous Glucose Monitors (CGMs)
Let’s talk about gadgets—because if you're serious about managing or understanding your blood sugar, you need the right tools. Glucometers are the classic go-to: a simple finger prick gives you a quick snapshot of your current glucose level. They're affordable, easy to use, and perfect for spot-checking your post-meal response.
Then there are Continuous Glucose Monitors (CGMs), the tech-savvy upgrade. These devices track your glucose 24/7 via a small sensor under your skin. They send real-time data to your phone or smartwatch, giving you a complete view of your glucose trends throughout the day and night. You can literally see the spike from that breakfast bagel or the flat line after a balanced salad.
CGMs are especially helpful for people with diabetes, but health enthusiasts and athletes are also using them to optimize energy and performance. They help you learn which foods work for your body and when your blood sugar tends to dip or spike—knowledge that empowers you to make smarter decisions.
Best Times to Check Postprandial Blood Sugar
Timing is everything when checking post-meal glucose. Most experts recommend measuring it at 1 hour and 2 hours after your first bite. Here’s why:
-
1 Hour Post-Meal: This typically shows the peak of your glucose rise. It tells you how high your blood sugar spiked.
-
2 Hours Post-Meal: This shows how quickly your body is bringing your sugar back down. Ideally, it should return close to your pre-meal (fasting) level.
If you’re new to this, try checking at both time points after different meals. You’ll quickly see patterns—like how pizza hits harder than a chicken-and-quinoa bowl. It’s like running an experiment on your own metabolism.
Blood Sugar Targets for Different Groups
For Non-Diabetics
If you don’t have diabetes, your post-meal blood sugar should generally stay below 140 mg/dL at the 1- or 2-hour mark. Your fasting glucose should hover between 70–99 mg/dL. If you're regularly above that—even without symptoms—it could be a warning sign of insulin resistance or prediabetes.
But here's the catch: many non-diabetics never check their post-meal sugar. And that’s a missed opportunity. Subtle imbalances can fly under the radar for years before turning into full-blown diabetes. Early tracking gives you a head start on prevention.
For People with Type 1 and Type 2 Diabetes
People with diabetes have different targets, usually set by their healthcare provider. That said, general post-meal goals are:
-
Below 180 mg/dL 1-2 hours after eating
-
Pre-meal target: 80–130 mg/dL
The key here is consistency. Occasional spikes are expected, but repeated high readings can damage blood vessels, nerves, and organs over time. Monitoring helps you adjust insulin doses, meal timing, and carb intake for better control.
For Pregnant Women with Gestational Diabetes
Gestational diabetes (GD) comes with its own unique challenges. Blood sugar control during pregnancy is crucial for both mom and baby. Guidelines usually recommend:
-
1-hour post-meal: < 140 mg/dL
-
2-hour post-meal: < 120 mg/dL
Even slight elevations can affect fetal development and lead to complications. That’s why frequent testing, a controlled diet, and exercise are often prescribed during pregnancy. And for many women, these habits stick around long after birth—setting the stage for a healthier life.
Tips to Keep Blood Sugar Stable After Eating
Eat Balanced Meals
Think of your plate like a team: carbs might be the star player, but they need good support from protein, fiber, and healthy fats to win the game. A balanced meal doesn’t just taste better—it digests slower, gives you lasting energy, and keeps your blood sugar from spiking and crashing.
Here’s what a balanced plate might include:
-
Protein: Chicken, eggs, tofu, fish, or legumes
-
Carbs (preferably complex): Sweet potatoes, whole grains, or brown rice
-
Fiber: Leafy greens, berries, lentils, or flaxseeds
-
Fats: Avocado, olive oil, nuts, or seeds
This combination ensures that glucose enters your bloodstream gradually. Plus, protein and fat increase satiety—meaning you’ll feel fuller, longer, and won’t crave a sugar fix 30 minutes later.
Avoid Sugary Beverages and Refined Carbs
You’ve probably heard this before, but it bears repeating: sugary drinks and refined carbs are blood sugar bombs. Soda, fruit juices, energy drinks, and even “healthy-looking” smoothies can send your glucose skyrocketing.
Refined carbs—like white bread, crackers, or pastries—have been stripped of fiber and nutrients. They turn into sugar almost instantly. The result? A quick spike followed by a crash, leading to fatigue, hunger, and cravings.
Instead, hydrate with water, herbal teas, or drinks like lemon water or infused cucumber-mint. These help flush out excess glucose and support digestion.
Include Fiber and Healthy Fats
Fiber is like nature’s glucose slow-release valve. It slows down digestion, delays glucose absorption, and supports healthy gut bacteria. Soluble fiber (found in oats, beans, flaxseeds) is especially effective at taming post-meal sugar.
Healthy fats, like omega-3s and monounsaturated fats, also reduce the glycemic impact of a meal. They don’t raise your blood sugar at all—and when paired with carbs, they create a smoother post-meal curve.
Try adding a drizzle of olive oil to veggies, a spoonful of nut butter to your oats, or a few slices of avocado to your sandwich. These small tweaks make a big difference in blood sugar management.
Sample Meal Plan for Better Postprandial Control
Breakfast, Lunch, Dinner, and Snack Examples
Let’s break down a day’s worth of meals that are blood sugar-friendly yet totally satisfying.
Breakfast
-
Scrambled eggs with spinach, tomato, and feta
-
1 slice of whole grain toast
-
A handful of berries
-
Green tea or black coffee
Lunch
-
Grilled chicken salad with mixed greens, quinoa, avocado, and olive oil vinaigrette
-
Sparkling water with lemon
Dinner
-
Baked salmon
-
Steamed broccoli and roasted sweet potato
-
A small mixed greens side salad with olive oil dressing
Snack
-
Greek yogurt with chia seeds and cinnamon
-
A few almonds
These meals combine protein, fiber, and healthy fats to keep your blood sugar stable throughout the day. They also taste amazing—because let’s be real, nobody wants to eat cardboard just to avoid a spike.
How Meal Timing Can Help
When you eat matters almost as much as what you eat. Eating your biggest meal at lunch can help reduce afternoon crashes and nighttime sugar spikes. Try to eat dinner at least 2–3 hours before bed to give your body time to digest and stabilize blood sugar before sleep.
Spacing your meals about 4–5 hours apart allows insulin levels to return to baseline. Grazing all day—or snacking late at night—keeps insulin elevated, which can lead to insulin resistance over time.
Pro tip: take a light walk after meals. Even 10–15 minutes of movement can lower your blood sugar by helping muscles absorb glucose more efficiently.
Common Myths About Blood Sugar After Eating
Carbs Are Always Bad
Let’s set the record straight—carbs aren’t your enemy. In fact, they’re your body’s primary energy source. The real issue? Refined carbs and excessive carbs. Whole-food carbs like fruits, veggies, legumes, and whole grains provide energy, fiber, and nutrients.
The key is balance and timing. Pair your carbs with protein and fat. Choose low-GI options. Watch your portions. That way, you get the benefits without the spikes.
Demonizing all carbs can backfire, leading to nutrient deficiencies and low energy. Instead of eliminating carbs, learn to master them.
Only Diabetics Should Monitor Post-Meal Sugar
False. Everyone can benefit from knowing how their body reacts to food. You don’t need a diagnosis to take charge of your health.
In fact, many people discover they’re prediabetic—or at risk—only after seeing abnormal post-meal spikes. Early awareness can spark lifestyle changes that prevent disease entirely.
Even for athletes, busy professionals, or health-conscious folks, post-meal tracking reveals how food, sleep, stress, and exercise affect energy, focus, and performance. Think of it as a tool for optimization, not just management.
Symptoms of High and Low Blood Sugar Post-Meal
Signs You Shouldn't Ignore
Your body usually gives off subtle (and sometimes not-so-subtle) clues when your blood sugar isn’t where it should be. After eating, if your glucose spikes too high, you might feel:
-
Fatigue or drowsiness
-
Blurred vision
-
Dry mouth
-
Excessive thirst
-
Headaches
-
Frequent urination
These symptoms can feel like a post-lunch slump, but they may actually be due to elevated glucose levels. Over time, repeated high readings can desensitize your body to these signs, making glucose testing even more important.
On the flip side, a drop in blood sugar after eating (reactive hypoglycemia) can cause:
-
Dizziness or shakiness
-
Sweating
-
Rapid heartbeat
-
Irritability
-
Brain fog or confusion
-
Sudden hunger, even after a full meal
If you experience any of these symptoms regularly, especially within 1 to 3 hours after eating, it’s wise to monitor your blood sugar and consult your doctor. Sometimes the symptoms seem random but are actually part of a predictable pattern.
When to Seek Medical Help
Occasional highs or lows are part of life, especially after eating a heavy meal or skipping physical activity. But if your post-meal readings are consistently above 180 mg/dL (for diabetics) or 140 mg/dL (for non-diabetics), you should consult your healthcare provider.
Likewise, recurring lows (under 70 mg/dL) after meals could indicate an issue with insulin production or timing—something that warrants medical attention.
Left unchecked, extreme glucose swings can lead to hypoglycemic episodes, fainting, seizures, or long-term complications. So don’t wait until things feel “serious.” When it comes to blood sugar, sooner is always better.
Long-Term Risks of Poor Postprandial Control
Cardiovascular Health
Poor blood sugar control after meals doesn’t just affect your energy—it can silently damage your heart and blood vessels. Chronically elevated post-meal glucose leads to inflammation and oxidative stress, which wear down the arterial walls and increase the risk of:
-
High blood pressure
-
Stroke
-
Heart attacks
-
Atherosclerosis (hardening of the arteries)
Even people without diabetes can face these risks if their post-meal glucose is routinely high. That’s why doctors now recognize postprandial hyperglycemia as an independent risk factor for cardiovascular disease.
Keeping your post-meal numbers in check is like giving your heart a daily tune-up—protecting it from wear and tear.
Risk of Developing Type 2 Diabetes
Here’s a harsh truth: most people don’t go to bed healthy and wake up diabetic. It’s a slow, creeping process—and post-meal sugar spikes are often the first clue.
If your body struggles to return to normal glucose levels after meals, it’s a sign that insulin resistance is setting in. Left unchecked, this can evolve into prediabetes and eventually full-blown type 2 diabetes.
But the flip side is empowering: by addressing postprandial control now—through diet, movement, and monitoring—you can reverse insulin resistance, lower your A1C, and reduce or even eliminate your risk of diabetes.
The Role of Stress and Sleep in Post-Meal Blood Sugar
Cortisol’s Impact on Glucose
Think stress is just mental? Not at all. It has a huge physical impact—especially on blood sugar. When you’re stressed, your body releases cortisol, a hormone that makes glucose more available so you can “fight or flee.”
The problem? If you're sitting at a desk worrying about work (instead of running from danger), that extra glucose has nowhere to go—so it lingers in your bloodstream. That’s why stress can raise your post-meal glucose significantly.
Chronic stress also increases insulin resistance, making it harder for your cells to absorb sugar after meals. Learning to manage stress through mindfulness, deep breathing, or even short walks can actually improve your blood sugar control.
How Poor Sleep Affects Insulin Sensitivity
Sleep isn’t a luxury—it’s a metabolic necessity. Skimping on sleep for even one night can reduce your insulin sensitivity the next day, causing your body to respond poorly to food.
In fact, studies show that just four hours of sleep can impair glucose tolerance by up to 40%. That means your body processes sugar like someone with prediabetes—even if you're otherwise healthy.
Make good sleep hygiene a priority:
-
Stick to a regular bedtime
-
Avoid screens before bed
-
Create a dark, cool, quiet sleep environment
Your glucose—and your mood—will thank you.
Natural Supplements and Herbs That May Help
Cinnamon, Berberine, and More
Looking for natural ways to support your post-meal glucose? Several supplements have been shown to improve insulin sensitivity and reduce blood sugar spikes. Here are a few to consider:
-
Cinnamon: A popular spice that can mimic insulin and slow glucose absorption. Ceylon cinnamon is safer for long-term use.
-
Berberine: Found in plants like goldenseal and barberry, this compound improves insulin sensitivity and reduces glucose production in the liver.
-
Alpha-lipoic acid (ALA): An antioxidant that enhances glucose uptake and may help with nerve symptoms in diabetics.
-
Chromium picolinate: Supports carbohydrate metabolism and may help regulate insulin response.
-
Fenugreek: A fiber-rich herb that slows digestion and blunts blood sugar rise.
What the Science Says
Many of these supplements have shown promising results in clinical studies, but they’re not magic bullets. They work best alongside a healthy diet, exercise, and sleep. Always talk to your doctor before starting a new supplement, especially if you’re on glucose-lowering medications, to avoid unintended drops.
Think of these as supportive tools—not replacements for lifestyle changes.
How to Talk to Your Doctor About Post-Meal Spikes
What to Track and Report
Your doctor can only help you as much as the data you bring them. If you suspect your post-meal blood sugar is off, track it consistently for 1–2 weeks. Record:
-
Time and content of meals
-
Glucose levels 1 and 2 hours post-meal
-
Symptoms (fatigue, headache, hunger, etc.)
-
Sleep and stress patterns
-
Any exercise or walking done post-meal
This information paints a complete picture of how your body responds to food and lifestyle, helping your doctor make accurate recommendations.
Useful Questions to Ask
-
"Are my post-meal levels within a healthy range?"
-
"Do I show signs of insulin resistance?"
-
"Would a glucose monitor or CGM be useful for me?"
-
"Should I adjust my meal timing or composition?"
-
"Is it worth testing for prediabetes?"
Be proactive. Don’t wait for a diagnosis to start optimizing your health. Doctors appreciate patients who are engaged, informed, and ready to take action.
Conclusion
Understanding your blood sugar after meals is like unlocking a secret window into your metabolic health. It's not just a number—it's a real-time feedback loop that shows how your body is handling the food you eat and the life you live.
Whether you're managing diabetes, trying to avoid it, or just want more energy throughout the day, paying attention to post-meal glucose is a game changer. It empowers you to make smarter food choices, time your meals wisely, and create daily habits that support stable energy, better focus, and long-term health.
Remember, you don’t have to overhaul your life overnight. Start small: swap soda for water, add protein to breakfast, take a walk after dinner. Track what works for you and build from there. The goal isn’t perfection—it’s progress.
FAQs
How soon after eating should I check my blood sugar?
Ideally, test at 1 hour and 2 hours after your first bite. The 1-hour reading shows the peak, and the 2-hour reading tells you how well your body is recovering.
Can exercise lower post-meal blood sugar spikes?
Absolutely. A brisk 10–15 minute walk after eating can significantly lower your post-meal glucose by helping your muscles use up more sugar.
Are post-meal crashes dangerous?
Yes, especially if they’re frequent. A sharp drop in blood sugar after meals (reactive hypoglycemia) may indicate insulin dysregulation and should be evaluated.
Is it normal to feel sleepy after meals?
Occasionally, yes. But if it happens often, it might be a sign of high postprandial sugar followed by a crash. Adjusting your meal content can help.
What’s the difference between fasting and postprandial sugar?
Fasting sugar measures your baseline glucose level after not eating for 8+ hours. Postprandial sugar checks how your body handles glucose after a meal.